Review of MassHealth member eligibility expected to take a year
| Published: 05-14-2023 5:00 PM |
BOSTON — State officials on Thursday offered a first glimpse into efforts to redetermine MassHealth members’ eligibility.
About six weeks into the process, which is expected to take a year, about 70,000 Massachusetts households have begun the process of assessing whether they still qualify for state-funded health insurance.
Hundreds of thousands people are expected to lose MassHealth coverage over the next year as federal coverage requirements in place since March 2020 expired on March 31. As the state redetermines eligibility for the first time since the pandemic began, those who lose coverage will need to find new health insurance plans. Budget writers on Beacon Hill are already factoring into their spending plans massive savings associated with lower MassHealth rolls.
About 50 percent of MassHealth members will be automatically renewed. The other half of the 2.3 million people enrolled in the program will be receiving a blue envelope containing forms to fill out with their current information, which MassHealth will use to determine if they still qualify.
The number of people that the state expects to be pushed off the plan has been a moving target. Estimates range from 300,000 people to more than 400,000 – the higher end of which the Senate Ways and Means Committee used to build its fiscal 2024 budget, freeing up $1.8 billion that is allocated elsewhere.
Since the federal protections ended March 31, over 50,000 MassHealth members have been renewed after completing redetermination requirements.
The redetermination program began ramping up its workforce in anticipation of the work checking the eligibility of those 2.3 million enrollees, and helping those who no longer qualify transition to other coverage.
MassHealth aimed to double the amount of customer service representatives in call centers to 320, hire an additional 100 workers to determine eligibility, 80 to 100 temporary employees to process applications, and use grants to scale up the certified application counselor workforce.
Article continues after...
Yesterday's Most Read Articles
 Orange man gets 12 to 14 years for child rape
Orange man gets 12 to 14 years for child rape
 Carol Doucette of Royalston receives $15,000 from Publishers Clearing House
Carol Doucette of Royalston receives $15,000 from Publishers Clearing House
 Wheeler Mansion in Orange to reopen as bed and breakfast
Wheeler Mansion in Orange to reopen as bed and breakfast
 Phillipston board opens talks on new police chief
Phillipston board opens talks on new police chief
 Royalston Selectboard mulls options for full-time police
Royalston Selectboard mulls options for full-time police
In total, this includes increasing staffing levels by about 500 people to support the MassHealth Customer Service Center capacity, application processing, and hearings, and a $5 million grassroots outreach campaign in partnership with the Health Connector and Health Care For All.
About six weeks into the process, the help center, MassHealth systems and outreach efforts are still operating as planned, said Elizabeth LaMontagne, MassHealth chief of staff.
Throughout April, all mailed and faxed application documents were processed in less than 48 hours with zero backlog, she said, and there has only been a slight increase in calls to their contact center. The program estimates less than 1 percent of calls were abandoned before a caller was able to be helped.
An outreach program in partnership with Health Care For All is targeting the 15 cities with the highest number of MassHealth members, where “redetermination outreach team members” have knocked on nearly 146,000 doors and spoken to 26,000 people about the process. MassHealth is working with 42 community-based organizations to do this door-to-door canvassing and host events to get the information out.
As some residents lose MassHealth eligibility, the Health Connector is hoping to transition them to low-cost coverage through one of its available plans.
“We know that the Connector is going to be a natural landing place for a lot of folks that may be losing MassHealth eligibility over the course of the next 12 months,” Health Connector Executive Director Audrey Morse Gasteier said in March. She added, “We’ve been really getting ready for this event for almost the whole three-year period, thinking about all the ways that we can be most responsive when this time period came upon us.”
Now about halfway into May, over 2,400 individuals have transitioned from MassHealth to Health Connector coverage for May, and over 900 have enrolled for June. This reflects about 27 percent of those who have so far been found eligible for a Health Connector plan after being redetermined out of MassHealth.
These early enrollment figures exceed forecasted enrollment in Health Connector coverage at this point in the redetermination process, but Health Connector Director of Policy and Applied Research Marissa Woltmann said these individuals represented a particularly “proactive” group of people.
“The majority of these individuals have proactively come to the system and made updates to their application in a way that fulfills their renewal requirements. They didn’t wait for that blue envelope to come to them. And as a result, we’re seeing what we understand to be a relatively high conversion rate,” Woltmann said on Thursday. “While enrollments are exceeding forecast at this point, I’ll note that we are expecting to potentially see different dynamics emerge as more individuals are selected for renewal.”
As the Connector anticipates more residents turning to them for coverage, the program is in the process of recruiting and hiring a nine-person mobile outreach team to travel to different parts of the state to assist residents with in-person enrollment assistance.

 With eye toward teaching firearm safety, Mahar’s Junior ROTC adding air rifles
With eye toward teaching firearm safety, Mahar’s Junior ROTC adding air rifles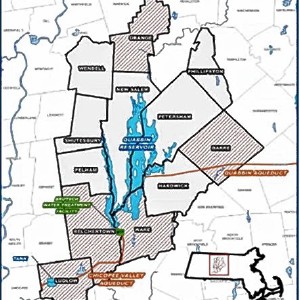 Quabbin region studied for MWRA expansion
Quabbin region studied for MWRA expansion Sportsman’s Corner: Quabbin opens this Saturday
Sportsman’s Corner: Quabbin opens this Saturday